Urologist and Author, Kelly Casperson emphasizes that testosterone transcends being solely a “male” hormone. It can play a crucial role in women’s health. Hormones intricately regulate various systems in the body, often leaving us uncertain about their specific functions or the reasons behind fluctuating hormone levels. This conversation gains prominence, particularly during perimenopause and post-menopause. Targeted hormone therapies become viable treatments for troublesome menopause-related symptoms. Symptoms like hot flashes, joint pain, low energy and diminished libido are improved when testosterone is added. While estrogen is the predominant hormone in hormone replacement therapy, we will turn the spotlight to testosterone.
Yes, we’re addressing the hormone commonly labeled as the “male” hormone. There are a lot of questions about hormone replacement therapy and we will answer a few of them today. We’ll discuss the benefits of adding testosterone treatment during menopause, how to get a prescription and why testosterone isn’t covered by insurance.

Women and Testosterone
Indeed, testosterone is present in women’s bodies, albeit at one-tenth the levels found in men’s bodies. It is also produced by the ovaries, which technically generate it at even higher levels than estrogen. As menopause sets in and the ovaries slow down, both estrogen and testosterone levels decrease. Similar to estrogen, testosterone treatment can be safely employed in hormone replacement therapy during menopause. However, this fact remains relatively unknown, as it is not extensively studied or officially FDA-approved for women.
Discover everything you didn’t know about testosterone in women, testosterone replacement therapy, and how to determine if it could be the suitable treatment for you during menopause.
The following portion of this article is from a recent article from Sheknows.com: Why Isn’t Testosterone FDA-Approved to Treat Menopause Symptoms? – SheKnows
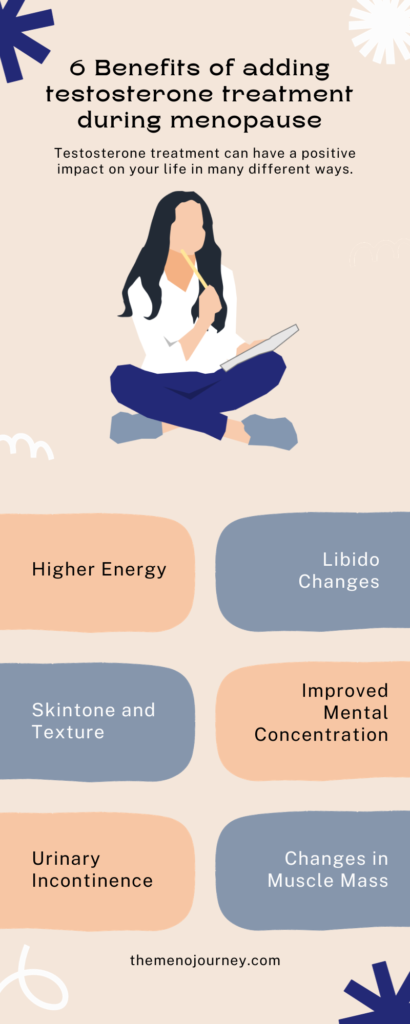
What are some of the benefits of testosterone treatment during menopause?
Testosterone has the potential to treat different menopause-related symptoms than estrogen. Here are some of its research-proven benefits:
Higher Energy
Fatigue, irritability, and a decreased feeling of well-being can be symptoms of low testosterone levels in pre- and post-menopausal women, according to a 2022 article. Another study that tested testosterone’s ability to treat musculoskeletal aches and pains, medically called arthralgias, actually found that taking testosterone over a period of months did not necessarily help the pain more than placebo, but did decrease fatigue and lessen mood swings.
Libido Changes
Androgens, a group of sex hormones that includes testosterone, are partially responsible for sexual desire, and androgen deficiency can lead to low libido during menopause. Research has shown that combining testosterone and estrogen therapy can result in the most improvement in libido.
Changes in Muscle Mass
Anecdotally, patients I have had who are on testosterone report gains in the gym. A small 2014 study also found that the women in the study given the highest dose of testosterone had higher lean body mass and muscle strength and had more power with chest presses and on stair climbing challenges.
Improved Mental Concentration
Believe it or not, menopause can affect your mental clarity, and testosterone might be able to help. Poor memory and focus can be signs of androgen deficiency, and some patients have reported greater mental clarity on testosterone therapy.
Skin tone and texture
Some patients who have excess androgens have reported increases in acne. But a recent study reported that women taking testosterone experience improvements in the smoothness of their skin tone and texture.
Urinary incontinence
Urinary health issues, including incontinence (bladder leakage), can be specific to pre- and post-menopause. These can be signs of a decrease in testosterone. The 2021 study intended to treat arthralgias also showed improvement in urogenital symptoms.
Out of Pocket Cost for Testosterone during menopause
To qualify for insurance coverage, there must be a designated testosterone product for women with both a specific FDA approval and recognized insurance reimbursement. Right now, testosterone is exclusively categorized as a men’s drug due to cultural perceptions. FDA approvals and dosing indications are tailored for men. The absence of FDA approval results in higher medication costs, rendering it less accessible. Despite the established safety of testosterone therapy for men, the FDA demands additional safety data for the women’s version, even though it involves only one-tenth of the dosage. Contrary to expectations, testosterone has been administered to women since the 1940s, accumulating substantial safety data over the years. This is unfortunate since the benefits of testosterone treatment can help women with their menopause symptoms.
Types of Testosterone treatment
There are four available formulations of testosterone: firstly, a topical gel, which is an FDA-approved male testosterone product costing approximately $20 per month out of pocket. Another option is a cream, which is slightly pricier. An injectable form is also available, although, less common due to the challenge of precisely measuring one-tenth of the dose administered to men. Testosterone pellets, implanted under the skin, represent another option. However, they are administered at higher doses and often associated with more side effects. Therefore, a doctor may initially recommend starting with the lower-dose gel before considering alternative options.
How to start a testosterone treatment
My OB/GYN prescribes my testosterone cream compounded with estradial. I use the cream every night on the back of my leg above my knee. I experienced side effects when I added testosterone treatment during menopause. Although a pain – they don’t keep me from using it and the benefits outweigh the problems. I’ll link a post here soon about the side effects of HRT with testosterone. I recommend asking your OB/GYN to run a hormone test at your next appointment to see if this would be an option for you.
The primary apprehension regarding testosterone use often revolves around estrogen-related cancers. In cases where patients are utilizing aromatase inhibitors to hinder the conversion of testosterone into potentially harmful estrogen, testosterone may be a viable and safe option. However, it is crucial to recognize that this decision is highly individualized. Before starting any treatment, it is imperative to consult with your medical care professionals.
This article is not a medical article nor does it provide medical advice, only an opinion based on my personal experience.